What states cap medical malpractice?
Medical malpractice insurance laws vary widely across the U.S., and for physicians, employers and healthcare organizations, those differences can have a direct impact on liability exposure, insurance costs and practice decisions. Understanding which states cap damages—and how those caps are evolving—helps medical professionals make informed career and coverage choices.
What states cap medical malpractice?
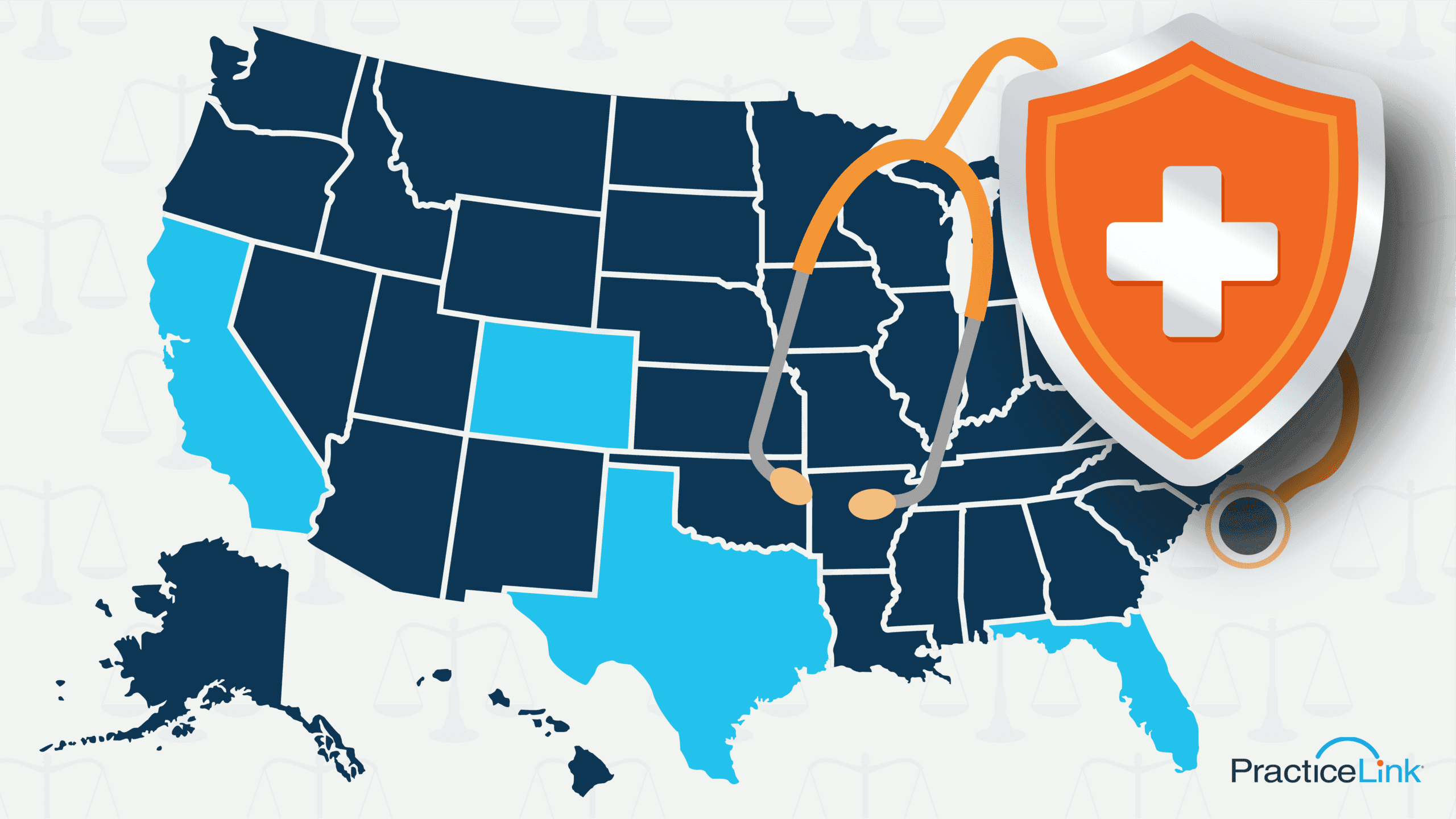
Medical malpractice caps limit the amount of money a patient can receive in a lawsuit, most commonly for noneconomic damages such as pain and suffering. As of 2025, the majority of states impose some form of cap, though the structure and dollar amount vary significantly. States such as California, Texas, Florida and Colorado are frequently cited examples, with caps designed to stabilize malpractice premiums and reduce excessive litigation.
Recent changes to state policies regarding caps on medical malpractice have been incremental rather than sweeping. Some states adjusted cap amounts to account for inflation, while others clarified how caps apply in cases involving multiple defendants or catastrophic injuries. A small number of states have ruled caps unconstitutional.
When examining medical malpractice by state, it becomes clear that caps alone do not tell the full story. States with caps often see more predictable insurance markets, but outcomes also depend on claims frequency, judicial climate and local healthcare infrastructure. For physicians comparing opportunities across state lines, caps are an important—but not exclusive—factor in assessing professional risk.
What state has the highest medical malpractice rate?
Determining which state has the highest medical malpractice rate depends on how “rate” is defined. Some analyses focus on claim frequency per physician, while others look at premium costs or payout totals. New York, Florida and Pennsylvania are among the states with highest malpractice insurance costs, driven by large populations, complex healthcare systems and active litigation environments.
From a workforce perspective, malpractice rates influence where physicians choose to live and practice. In states where malpractice risk is perceived as high, insurance premiums rise, increasing overhead for physicians. This can discourage doctors from practicing in those areas, contributing to shortages—particularly in high-risk specialties such as obstetrics and surgery. To compensate, salaries may increase, but higher income does not always offset the stress and cost associated with elevated liability exposure.
What is the best state for doctors medical malpractice?
The “best” state for doctors in terms of malpractice is typically one that balances reasonable liability protections with a stable legal environment. States with clear caps, predictable court rulings and lower claim frequency tend to rank favorably. Texas is often cited due to its long-standing cap on noneconomic damages. Midwest and Mountain West states also perform well in comparative studies.
Looking at medical malpractice statistics by state, favorable states generally show lower average premiums, fewer claims per physician and shorter case resolution timelines. These factors contribute to reduced stress and lower operating costs for medical practices. Importantly, states with supportive malpractice environments often see stronger physician retention and recruitment, benefiting both providers and patients.
What states are most litigious for medical malpractice?
Litigiousness refers to how frequently malpractice claims are filed and how aggressively they are pursued. States commonly viewed as highly litigious include New York, Florida, New Jersey and Illinois. These states tend to report higher medical malpractice payouts by state, driven by large jury awards and higher claim volumes.
In response, 2025 changes to state policies regarding medical malpractice tort have focused on procedural reforms rather than outright caps, including:
- Strengthened pre-trial screening panels
- Modified expert witness requirements
- Adjusted statutes of limitation.
These reforms aim to reduce frivolous claims while preserving patients’ rights to pursue legitimate cases.
Higher litigation risk can affect not only insurance costs but also practice style, leading to more defensive medicine and increased administrative burden.
Medical malpractice caps and litigation trends can shape insurance costs, physician supply and overall healthcare access. Whether you are comparing opportunities, evaluating risks or planning long-term career moves, understanding how malpractice laws work at the state level is essential.
For deeper insights, expert guidance and physician-focused perspectives, explore PracticeLink’s Resource Center, where you’ll find physician-first articles, podcasts and strategic partners to support you at every stage of your medical career.

